WHAT IS A GLAUCOMA?
Glaucoma is the name given to a group of diseases which all have the final outcome of damaging the optic nerve (which sends signals from the retina in the eye to the brain) and permanently impairs peripheral vision and sight. It is the leading cause of irreversible blindness world wide.
What Does a Damaged Optic Nerve Look Like?
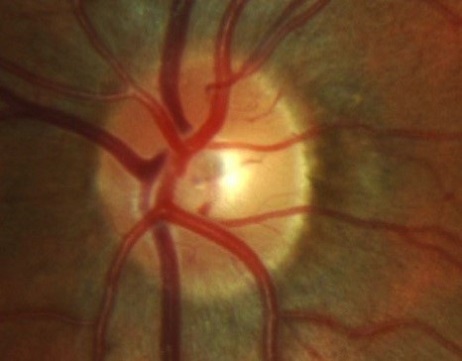
Normal Eye
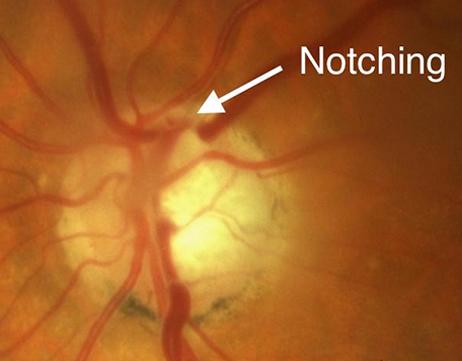
Glaucomatous optic nerve
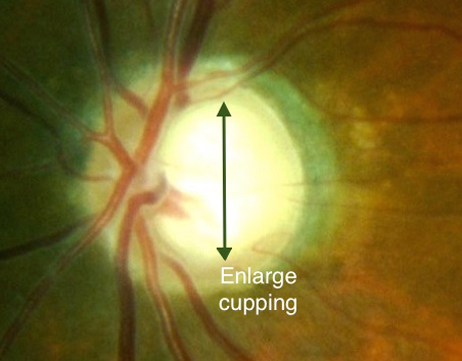
Enlarge Cupping
Above are 3 different optic nerves photos. The one on the far left is normal.
The one in the middle demonstrates a glaucomatous optic nerve with localised loss of nerve tissue in the upper part of the nerve resulting in the appearance of a ‘notch’. The picture in the far right has generalised enlarged ‘cupping’ of the nerve. The enlarging central cup is absent of any nerve fibres while the nerve rim which contains optic nerve fibres progressively thins out and becomes pale and transparent.
WHAT CAUSES GLAUCOMA?
Primary open angle glaucoma (POAG) is the most common form of glaucoma in Australia. The most important risk factor for developing glaucoma is the presence of elevated internal eye pressure (intraocular pressure). Fluid is constantly produced within the eyeball and this fluid (aqueous humor) is constantly drained out of the eye via the trabecular meshwork – a spongy tissue located where the cornea and iris meet (see picture). When aqueous humor is drained too slowly out of this meshwork, fluid within the eye builds up and internal eye pressure rises.
Other risk factors associated with open angle glaucoma include:
- Family History: First degree relatives of glaucoma patients have a 4 to 8-fold increase in developing glaucoma. Early screening for glaucoma is recommended for those with a strong family history of the disease and for first degree relatives of glaucoma patients.
- Age: POAG becomes much more common with increasing age. Whilst it is uncommon below the age of 40, incidence rises steadily with age affecting 10% of Australians over the age of 80.
- Ethnic background: Those of African-Caribbean origin are four times more at risk of POAG than a person of Caucasian descent, and it may also come on at a younger age and be more severe. People of Asian descent are more likely to develop another type of glaucoma – namely ‘angle closure glaucoma’.
- Other risk factors include high short sightedness, cardiovascular disease, migraine and diabetes. Those with previous eye conditions and trauma as well as long term use of corticosteroids may develop a form of secondary open angle glaucoma.
WHAT ARE THE SYMPTOMS OF GLAUCOMA?
Glaucoma is sometimes called the ‘silent thief of sight’ as early stages of the disease are completely without symptoms. Peripheral (side) vision is damaged initially with gradual progression of visual field loss towards central vision. As such, by the time a patient is aware of their vision loss, the disease is usually quite advanced. Patients with advanced glaucoma have very little peripheral vision and may seem to be looking through a tunnel, often missing objects to the side. Over time, even central vision will be affected until no sight remains. Unfortunately, vision loss from glaucoma is not reversible with treatment, hence early diagnosis and treatment is the key to prevent / slow down the progression of visual field loss during early stages of the disease.
HOW IS GLAUCOMA DIAGNOSED?
In general, diagnosis of primary open angle requires assessment of multiple clinical parameters such as:
- Optic nerve appearance
- Intraocular pressure
- Results from several investigative tests
Common tests that you will have include visual field tests. Please see adjacent example glaucomatous visual field plot and OCT scanning of your optic nerve. For more information on OCT scan, please click here.
In some patients, the presence (or absence) of glaucoma can only be determined after a period of follow-up and repeated clinical examination and tests.
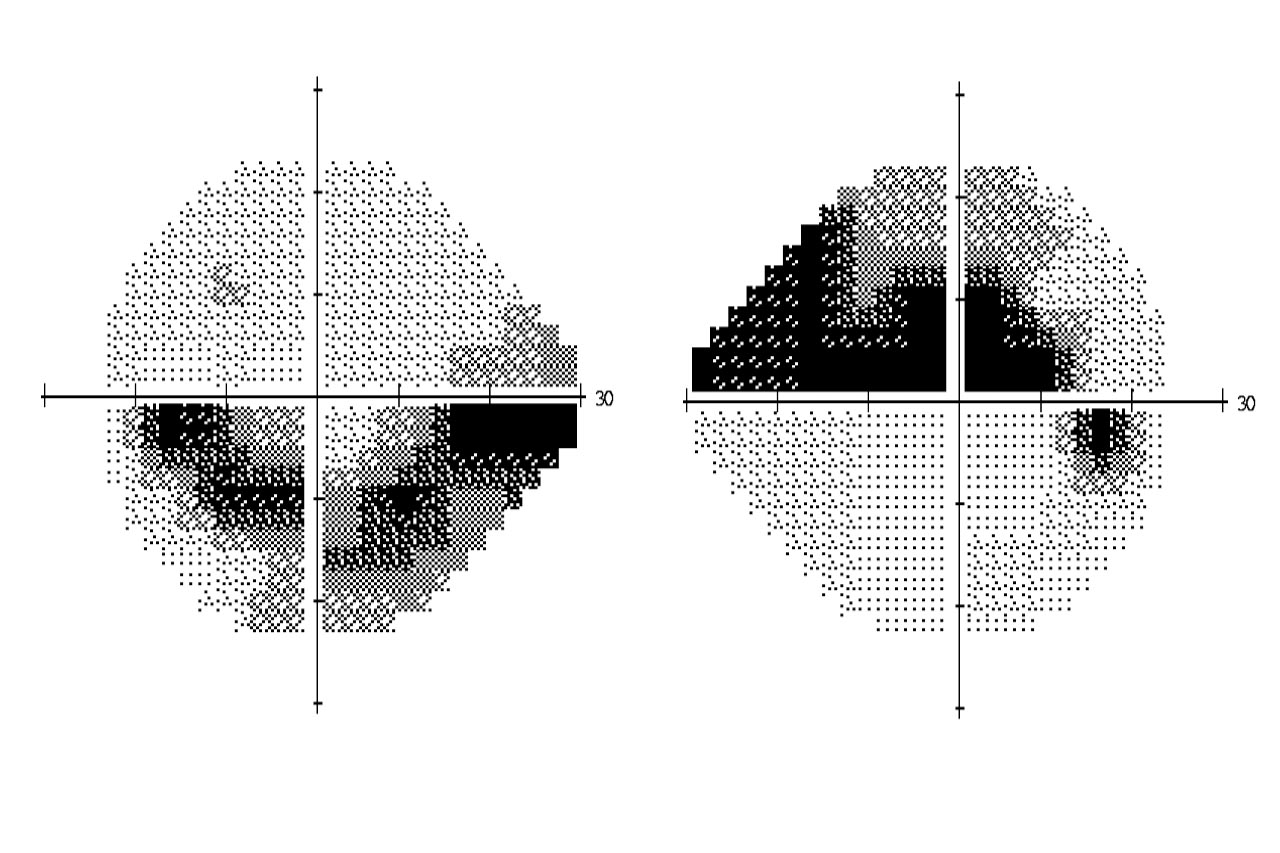
This is a plot of the typical peripheral visual field loss from a patient with bilateral glaucoma. The picture on the left demonstrates ‘arcuate’ loss in the lower half of the peripheral vision whilst the right had similar loss in the upper half of the vision.
TREATMENT FOR GLAUCOMA?
Whilst there is no ‘cure’ for glaucoma, treatment can slow down its progression. Almost all treatments focus on lowering the pressure in the eye.
Eye drops: Taken regularly, glaucoma eyedrops lower eye pressure by either causing the eye to make less fluid or by increasing the drainage of the fluid from the eye. Because glaucoma often has no symptoms, people may be tempted to stop or forget to instill the drops regularly. As such, it is important that glaucoma patients comply with the regular and long term use of the medications.
Peripheral iridotomy: This is a laser procedure which is used in some forms of glaucoma. Please click here for more information.
Selective Laser trabeculoplasty: This is a relatively new form of laser for glaucoma and is performed in the clinic. It can be used as an alternative or an adjunct to eye drops. Please click here for more information.
Surgery: Most patients with glaucoma do not need surgery. There are several types of surgery for glaucoma and they all work by enhancing the drainage of fluid from the eye. More information about glaucoma surgery can be found here.
HOW DO YOU MONITOR GLAUCOMA?
Primary open angle glaucoma is a ‘life-long’ disease that requires ongoing monitoring. Even when the intraocular pressure responds well to initial treatment, it can gradually increase over a number of months to years requiring additional treatment. In other patients, glaucoma damage may continue to occur despite a seamingly reasonable intraocular pressure reduction. In these cases, more aggressive intraocular pressure lowering may be required. Hence it is essential that clinical examination and testing be repeated on a regular basis to ensure that the glaucoma does not progress significantly.
With early detection, treatment and regular follow-up of primary open angle glaucoma, it is now uncommon for patients to become ‘blind’ or significantly affected by their glaucoma in their life-time.