What is diabetic retinopathy?
Diabetes affects the eye by damaging very small blood vessels (capillaries) in the retina (which is the thin membrane at the back of the eye responsible for sensing light). Over time, effects of diabetes cause these retinal capillaries to block up, leak fluid and bleed. This eventually leads to more abnormal, fragile blood vessels to grow in the retina, causing severe haemorrhage inside the eye, scarring, tractional detachment of the entire retina and blindness.
During early stages of diabetic retinopathy, there are often no symptoms at all. As such it is vital that regular retina checks be done (at least every 2 years even if no sign of diabetic retinopathy is found). Visual symptoms from diabetic retinopathy include: progressive blurring, patchy vision, sudden visual loss and floaters.
Unfortunately, diabetic retinopathy is still a leading cause of irreversible vision loss amongst working age Australians (25-75yro). Blindness from diabetes can be easily preventable through good diabetic control, regular monitoring of the retina and appropriate treatment when required.
What are the types of diabetic retinopathy?
Broadly speaking, diabetes causes two distinct clinical entities which have slightly different treatment strategies.
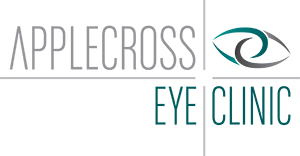
- Diabetic maculopathy: Diabetes can cause swelling and protein deposits in the central part of the retina (called the macula) which is responsible for our central vision including our ability to distinguish fine detail, read, drive and recognise faces. (Fig 1 and 2).
- Diabetic (peripheral) retinopathy: Diabetes can affect the peripheral part of the retina. It begins as non-proliferative diabetic retinopathy (NPDR), which does not require treatment (Fig 3), but can progress to proliferative diabetic retinopathy (PDR) which is a severe disease with a high risk of causing significant visual loss if left untreated (Fig 4).
Figure 1.
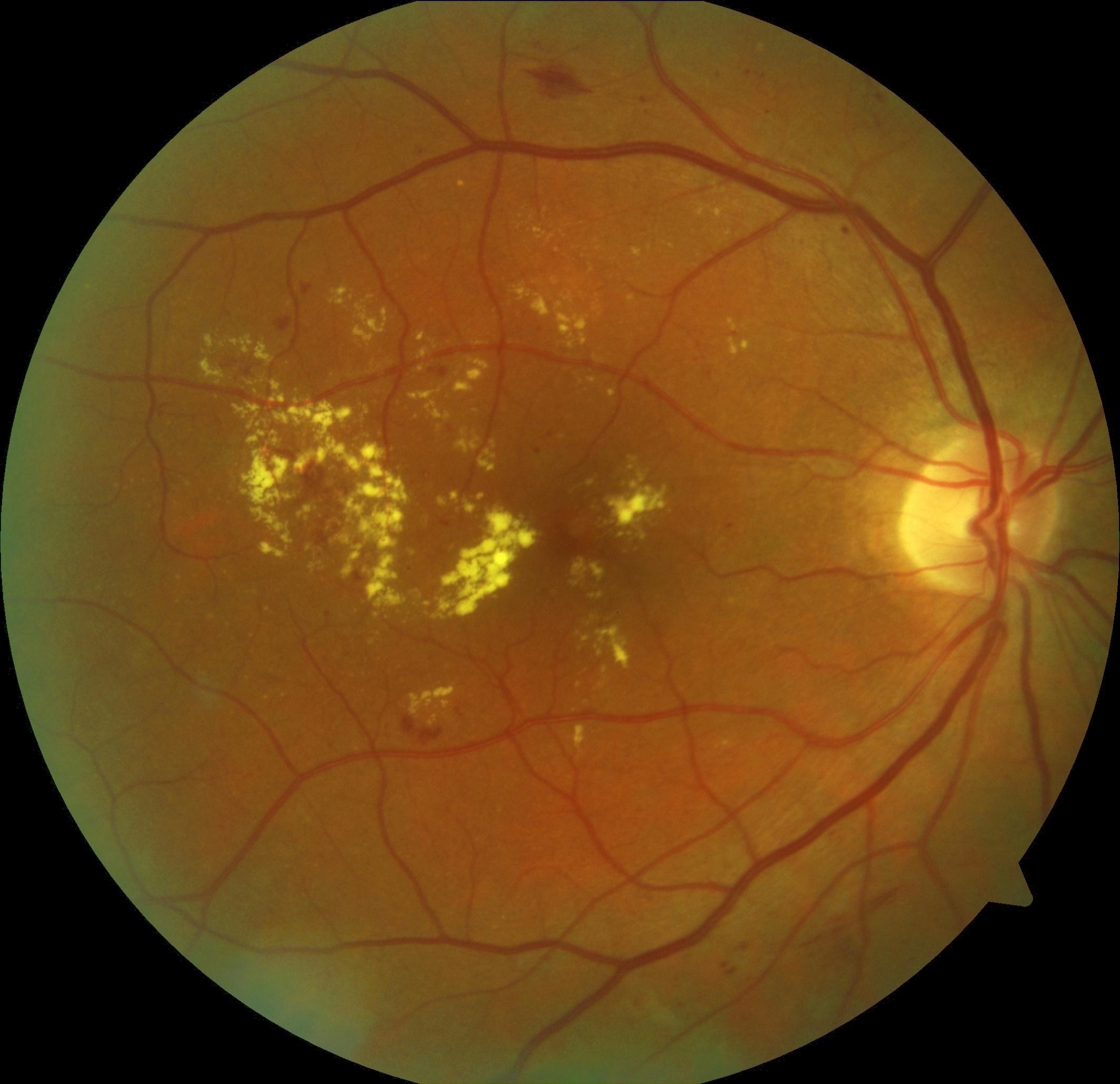
Fig 1: This patient has significant diabetic maculopathy with deposit of ‘hard exudate’ – the yellow spots at the centre of the macula and thickening of the macula.
Figure 2.
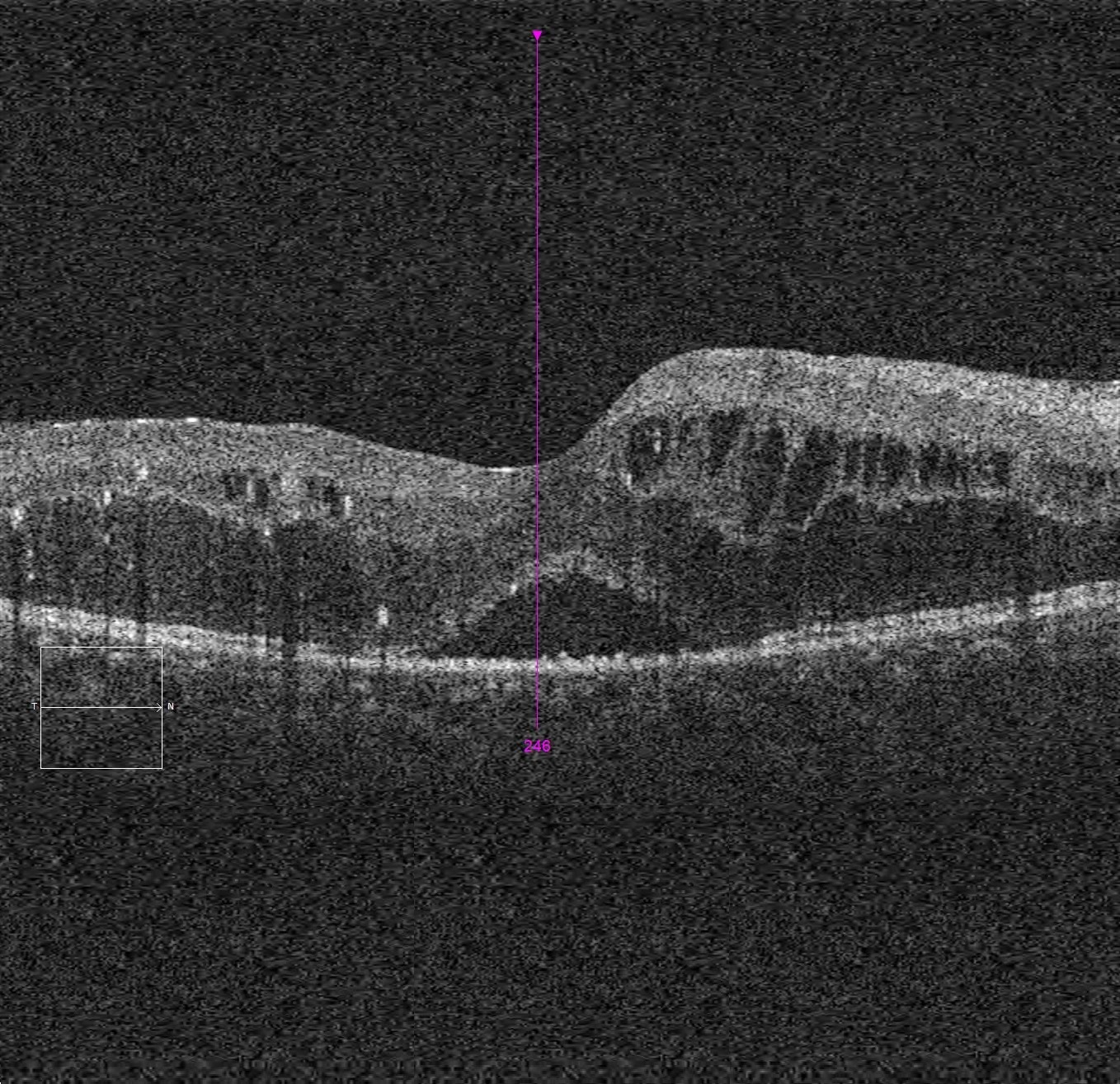
Fig 2: The OCT of this patient shows significant thickening and distortion with cystic changes within and under the retina.
Figure 3.
Fig 3: This patient’s retina starts off demonstrating signs of severe NPDR. There is presence of haemorrhage, micro-aneurysm and ‘cotton wool spots’ which represent areas of retinal infarct.
Figure 4.
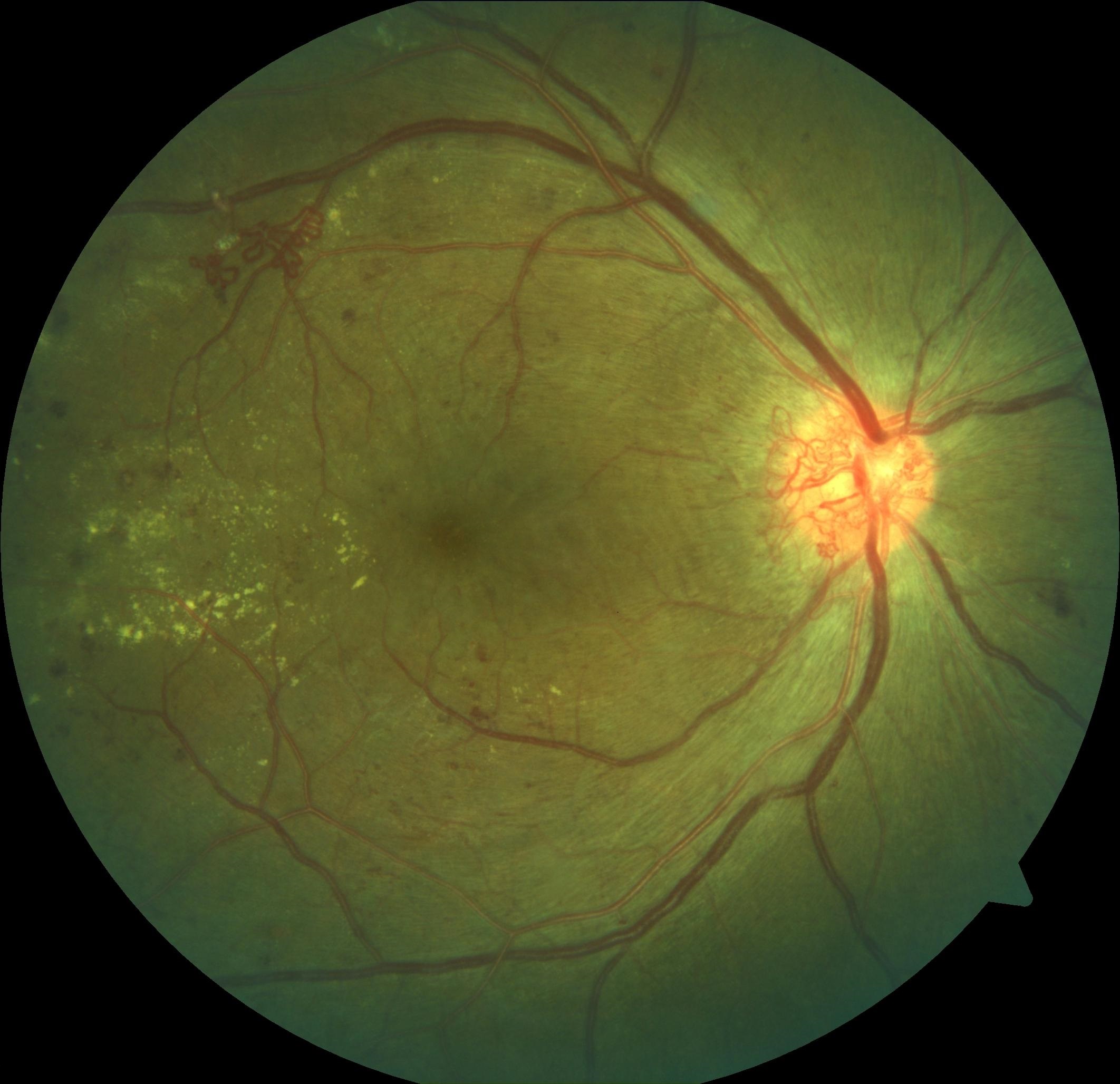
Fig 4: The patient in Figure 3 eventually developed PDR. In this picture there are ‘new vessels’ at the optic disc which are abnormal and are prone to bleeding and causing scar contraction.
What are the risk factors for developing diabetic retinopathy and losing vision from it?
Unfortunately, the longer the time one has had diabetes, the more likely diabetic retinopathy will occur. Almost everyone with type 1 diabetes and about 60% of those with type 2 diabetes will have some signs of diabetic retinopathy after 20 years.
Poor blood sugar control is a well-known risk factor. A number of large clinical trials have confirmed that those with well-controlled blood sugar levels do much better, with significantly lower risk of requiring treatment for their diabetic retinopathy and of developing blinding complications.
Other modifiable factors to reduce the risk of development and progression of diabetic retinopathy include having better control of high blood pressure, control of high blood cholesterol level, doing regular exercise, healthy eating, avoiding smoking and being overweight.
What are the treatments of diabetic retinopathy?
As mentioned above, good control of diabetes, blood pressure and blood cholesterol is vital in reducing risk of progression of diabetic retinopathy at any stage of the disease.
If treatment is required, it depends on which type of retinopathy is present:
For diabetic maculopathy with centre-involving macular swelling, the mainstay of treatment is the use of certain medication injected into the eye. Multiple injections are often required to achieve / maintain the best possible vision. Retinal laser can be useful in specific cases where the maculopathy is caused by a small area of leakage well away from the macular centre. A patient with maculopathy can self-monitor their central vision with the Amsler grid for early detection of macular damage.
For peripheral retinopathy, retinal laser remains as the primary treatment modality. To complete treatment to the entire peripheral retina, several thousand laser shots are required. This is usually performed over several treatment sessions for better tolerability and reduce the chance of potential side effects.