WHAT IS AGE-RELATED MACULAR DEGENERATION (AMD)?
Age-related macular degeneration is a condition where degenerative changes in the macula causes progressive, painless loss of central vision. Whilst AMD by itself will never cause complete ‘blindness’, it does affect the ability to see fine detail, drive, read and recognise faces but peripheral navigational vision is always preserved.
AMD typically occurs in older people and is the leading cause of severe vision impairment in people aged over 40 years in Australia. Although there is no ‘cure’ for AMD, treatments are available that can slow down its progression, depending on the stage and type of the disease.
WHICH PART OF THE EYE IS AFFECTED IN AMD?
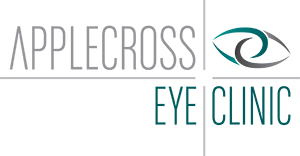
AMD damages the ‘macula’- which is a small area of the retina that is responsible for our central vision. Think of the eye as a camera. The front of the eye acts as a lens, focussing the image onto a thin membrane called the retina which lines the back of the eye and works like the film in a camera. (Fig 1). The retina itself in turn contains different cellular layers that are all important in producing sight (Fig 2). AMD begins with degeneration of cells in a certain layer of the macula, namely the Retinal Pigment Epithelium or RPE. Ultimately, it leads to progressive destruction and distortion of the remaining delicate cellular layers within the macula resulting in impairment of central vision.
Figure 1
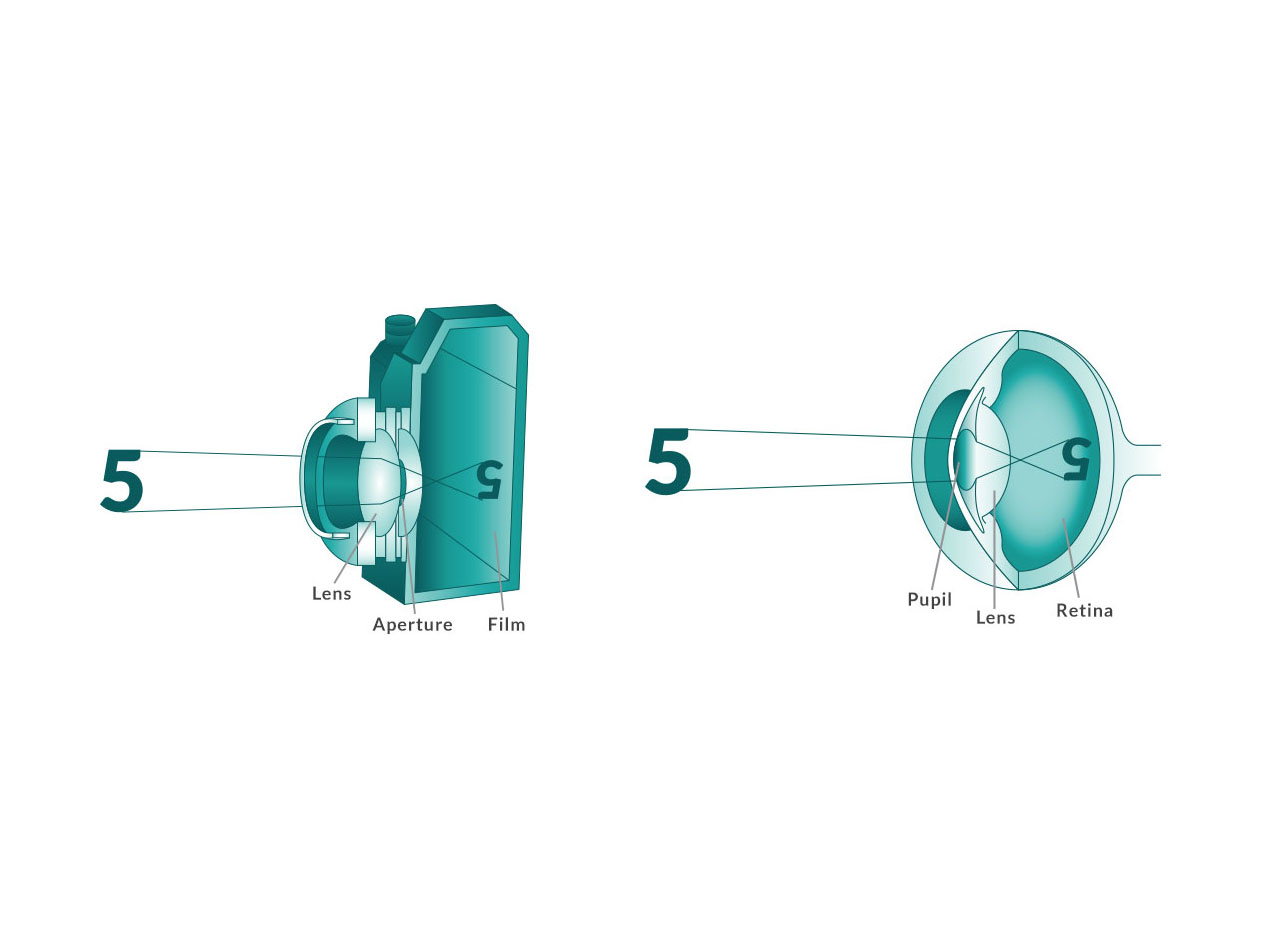
Figure 2
WHAT ARE THE TYPES OF AMD?
There are 2 types of AMD: dry macular degeneration and wet macular degeneration
DRY MACULAR DEGENERATION
This is the more common form of AMD. Approximately 90% of AMD patients have the dry form only. This is the slower form of the disease and causes gradual deterioration in vision over many years. The majority of people with dry AMD maintain a reasonable amount of vision during their lifetime. However, a small proportion of patients will convert to the ‘wet’ form (see below) which causes very rapid deterioration of vision. This conversion to wet AMD can occur at any stage of the disease. As such, it is important for patients with dry AMD to monitor their central vision regularly and report any sudden change in vision, distortion or new blind spots.
Below is a picture (Fig 3) showing typical signs of dry AMD. The yellow patches are called ‘drusen’ which are formed by accumulation of waste products underneath the retina. There are also ‘clumping’ of RPE cells and areas of ‘atrophy’ where the overlying retina have thinned out and died.
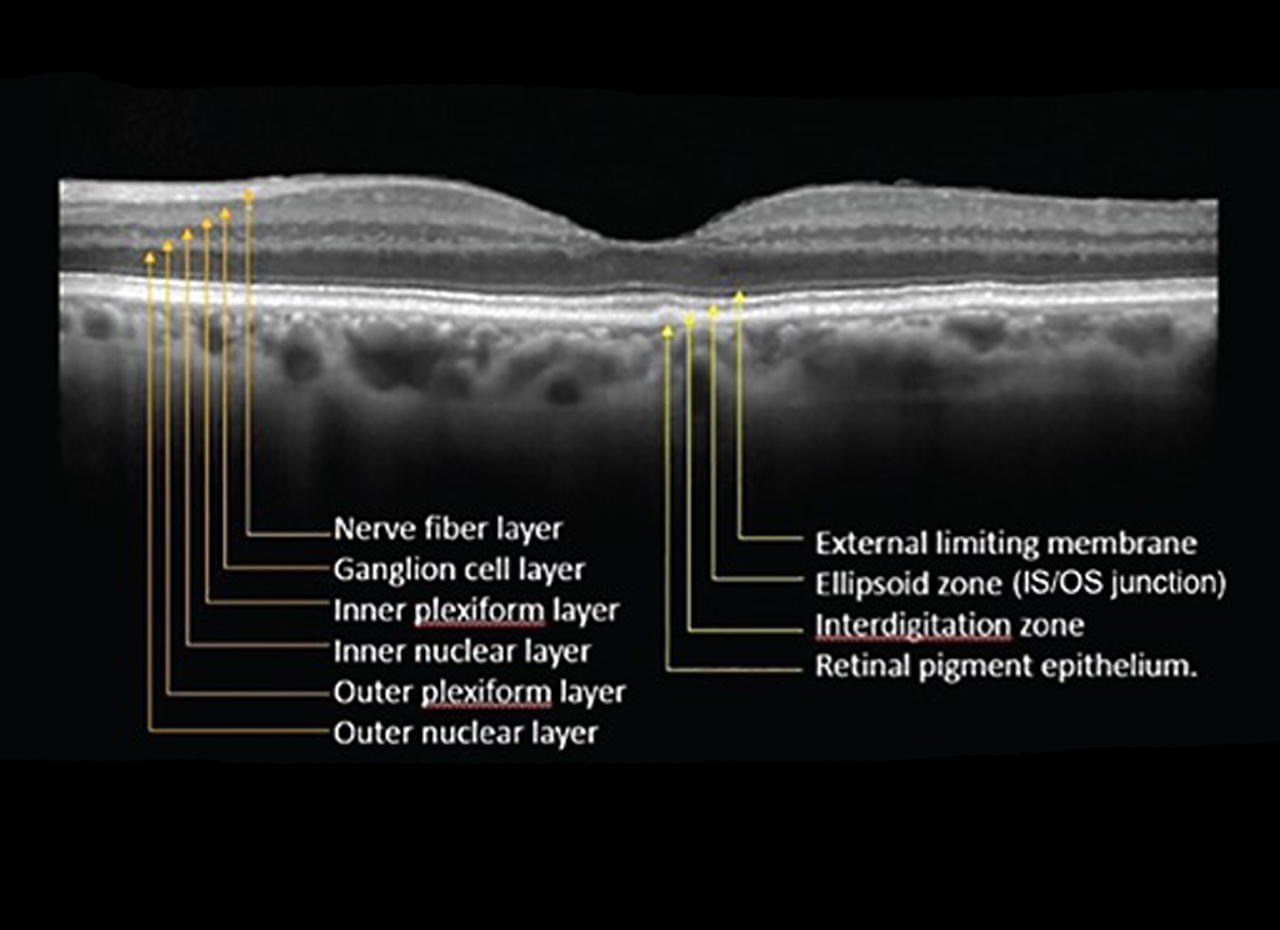
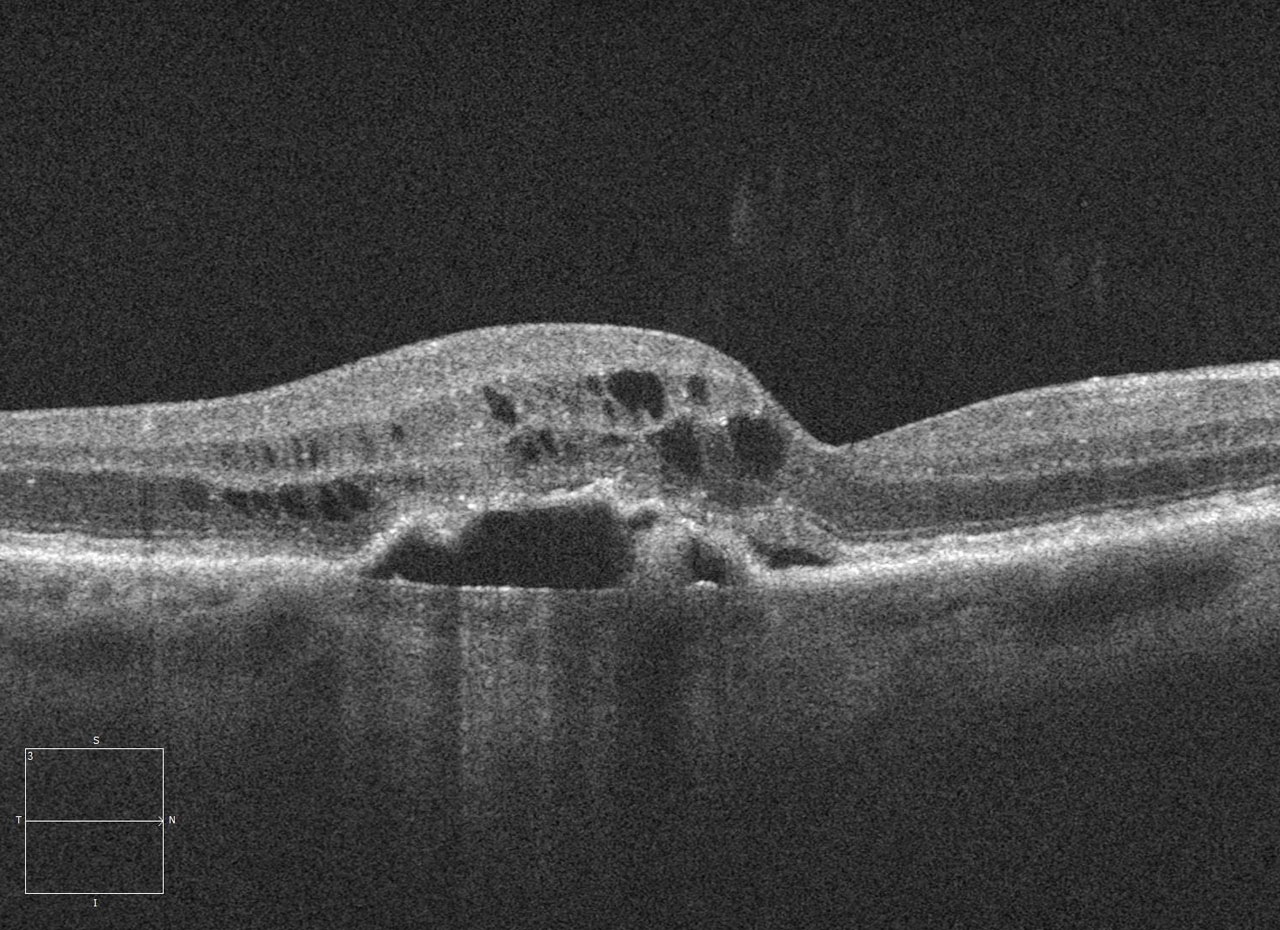
Figure 4 demonstrates a cross sectional scan using OCT technology of the macular region.
Figure 3

Figure 4
WET MACULAR DEGENERATION
Approximately 10% of AMD patients develop the ‘wet’ form of the disease during their lifetime. In addition to all the features of dry AMD, those with the ‘wet’ form develop abnormal blood vessels that grow from the choroidal layer underneath the retina through weakened areas in the RPE / Bruch’s membrane (which normally act as natural barriers). Think of it as tree roots surfacing through cracked pavements. Once these blood vessels surface into the sub-retinal space, they can cause serious damage to the overlying retina by leakage of fluid, bleeding and ultimately resulting in permanent macular scarring and loss of vision.
This process can occur relatively quickly, causing symptoms such as distorted / wavy vision, new blind spots and/or rapid deterioration of vision over days to weeks. As such, these symptoms should not be ignored, and prompt medical attention should be sought. Treatment consisting of regular injections into the eye needs to be started to prevent irreversible visual loss.
The picture below (Fig 5) shows a haemorrhage in the macula in a patient with wet AMD.
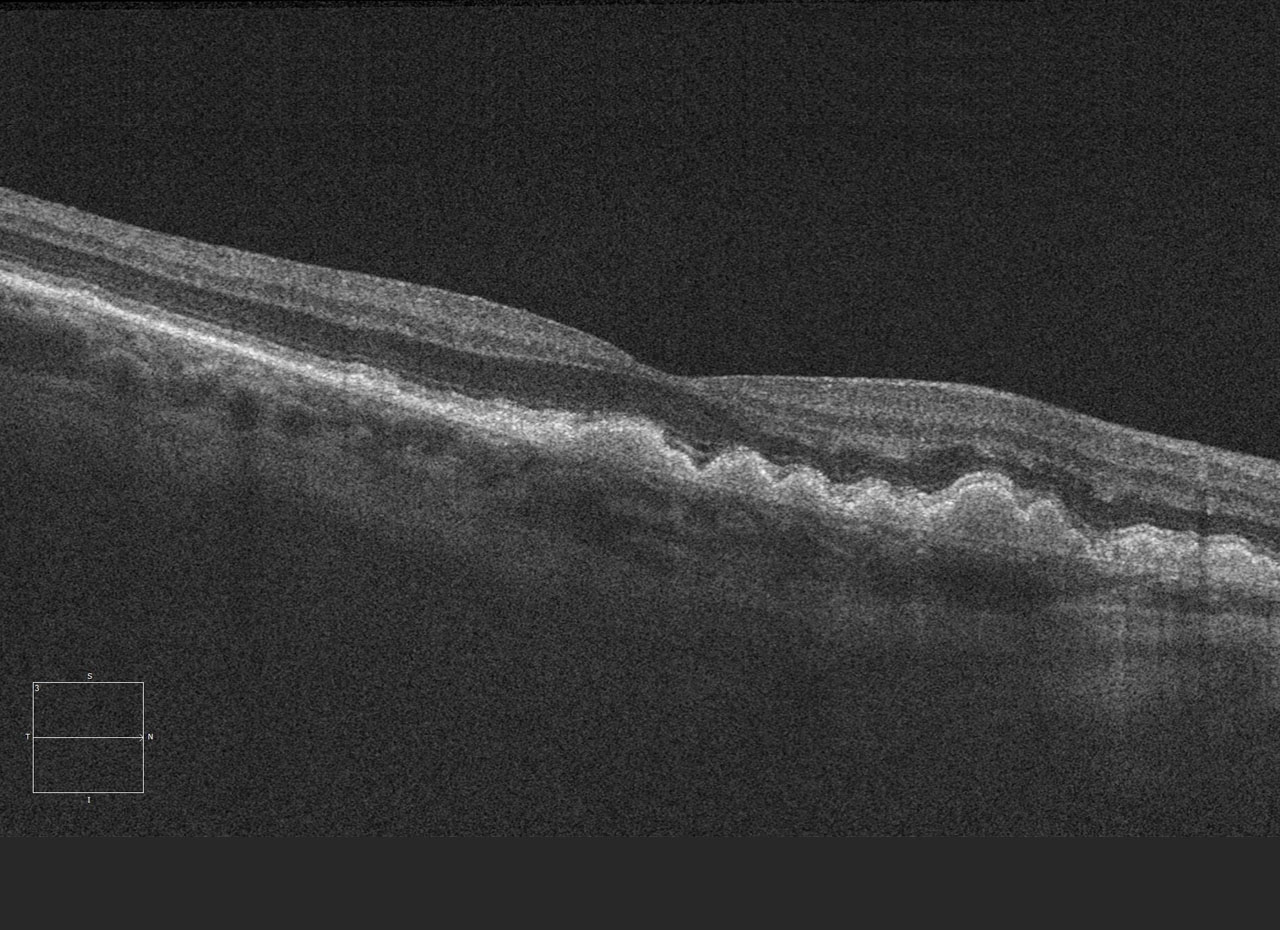
Figure 6 is an OCT scan of a patient illustrating leakage of fluid underneath the retinal layers causing distortion and elevation of the retina. This scan confirms the diagnosis, and is useful for ongoing monitoring of the progress of treatment.
Figure 5
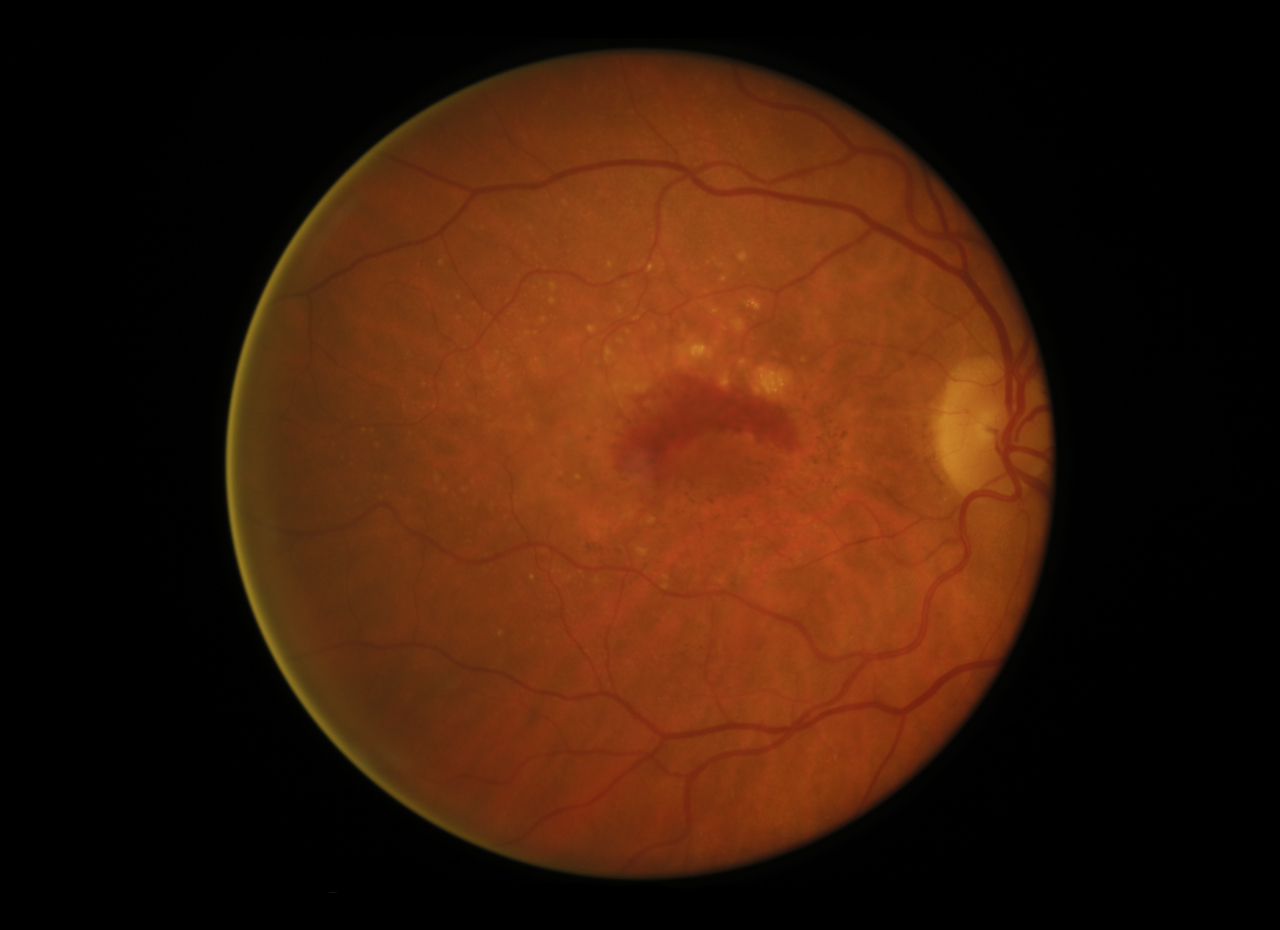
Figure 6
WHAT ARE THE RISK FACTORS?
Age: Age is a major risk factor for AMD. It is rare before the age of 50. Incidence rises sharply with age with approximately 1 in 7 Australians over 50 showing some sign of AMD. Over 14% of people over 80 have vision loss or blindness from AMD.
Family History and genetics: Those with a family history of AMD are at a higher risk of getting the same. A known first degree relative with AMD translates to a risk as high as 50% in developing the disease.
Other modifiable risk factors include:
- Smoking: those who smoke are 3-4 times more likely to develop AMD, and on average develop AMD 5-10 years earlier. 20 years after quitting, an ex-smoker’s risk is the same as someone who has never smoked.
- Vascular risk factors such as abnormal cholesterol, obesity, elevated pulse pressure
- UV exposure
WHAT TREATMENTS ARE AVAILABLE FOR AMD?
Unfortunately, there is no cure yet for either dry or wet AMD. Even for wet AMD, medical treatment consisting primarily of regular intravitreal injections in the eye aims only to stabilise the ‘wet’ form back into the dry form by causing regression of the abnormal blood vessels under the retina and stopping it from producing rapid visual loss.
Nutritional supplements have been shown in large clinical trials (such as the AREDS-1 and AREDS-2 trials) to help reduce the progression of AMD in some patients. However, they are not necessarily recommended for use in all patients with signs of AMD or those with family history only. Formulations based on compositions as tested on the above-mentioned clinical trials are readily available over the counter at any chemist or selected health food stores.
Other lifestyle changes in minimising the risk of further progression of AMD include cessation of smoking which increase the risk of blindness from AMD by up to 400%. Dietary changes to include plenty of green leafy vegetables, fish and a handful of nuts is also considered beneficial in slowing the progression of AMD.
It is also important to monitor one’s central vision regularly with the use of an Amsler grid. Click here for more information regarding how to monitor your vision for macular degeneration. It is also advisable to visit your optometrist for regular eye checks as early awareness and treatment is important in preventing permanent sight loss from AMD.
For further information about Age related macular degeneration, please consult one of our doctors at Applecross Eye Clinic.